ADHD in Kids: When Hyperactivity Breaks the Norm

ADHD has many faces: some children keep making careless mistakes and have trouble paying attention, some are overly active, and some are too shy and can hyperfocus on a specific activity. ADHD signifies a special way of brain functioning, but this way has many facets. Let’s learn about children ADHD, its main types, and other mental health conditions that often come along.
Key Takeaways
- Attention Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental condition that affects how children focus, behave, and learn.
- ADHD symptoms can include inattentiveness, hyperactivity, impulsivity, or a combination of these behaviors. Symptoms of ADHD can appear by age four, and early diagnosis can improve a child’s psychological and physical development.
- ADHD is thought to be largely genetic, with a heritability rate of about 80%. The exact cause is unknown but involves neurotransmitter imbalances.
- ADHD is categorized into three types: inattentive, hyperactive-impulsive, and combined.
- A diagnosis of ADHD should be considered if symptoms persist for more than six months and affect the child’s ability to function in various settings.
- Other conditions like learning disabilities, Oppositional Defiant Disorder (ODD), Conduct Disorder (CD), and Sensory Processing Disorder (SPD) often co-exist with ADHD.
- Treatment for ADHD typically involves behavioral therapy, parenting skills training, and sometimes medication. Physical activities and structured environments are proved to help manage ADHD symptoms effectively.
- Children with ADHD can lead normal lives with the right diagnosis, treatment, and support from parents, educators, and healthcare providers.
What is Attention Deficit Hyperactivity Disorder (ADHD)?
ADHD is diagnosed in around 3.3 million children in the US. It’s not an epidemic, and it’s definitely not contagious. The preferred term for people with ADHD is neurodivergent, which defines someone whose brain develops and works differently from those who are neurotypical.
If you’re looking for a medical term for ADHD, then it belongs to the class of neurodevelopmental disorders, together with autism spectrum disorder, motor disorders, and developmental learning disabilities.
As it’s a genetic disease, its first symptoms are already revealed by the age of four. With ADHD diagnosed at an early age, children have much higher chances of normal psychological and physical development.
What’s the cause of ADHD?
All the causes of ADHD remain unknown. However, numerous studies have found that it has to do with a genetic imbalance of neurotransmitters in the brain. More specifically, the neurotransmitters in the ADHD brain don’t communicate to neurons when to turn on and off the mode responsible for deep concentration and focus and when to switch to the mode of idling and resting. For neurotypical people, those two modes are alternating, while for ADHD people, they’re firing at the same time.
Also, the heritability of ADHD is around 80%, according to a recent study. And while ADHD experts still argue about the genetic mechanisms responsible for heritability, the fact that one of the parents has ADHD is one of the most significant risk factors for a child.
ADHD in children: symptoms and types
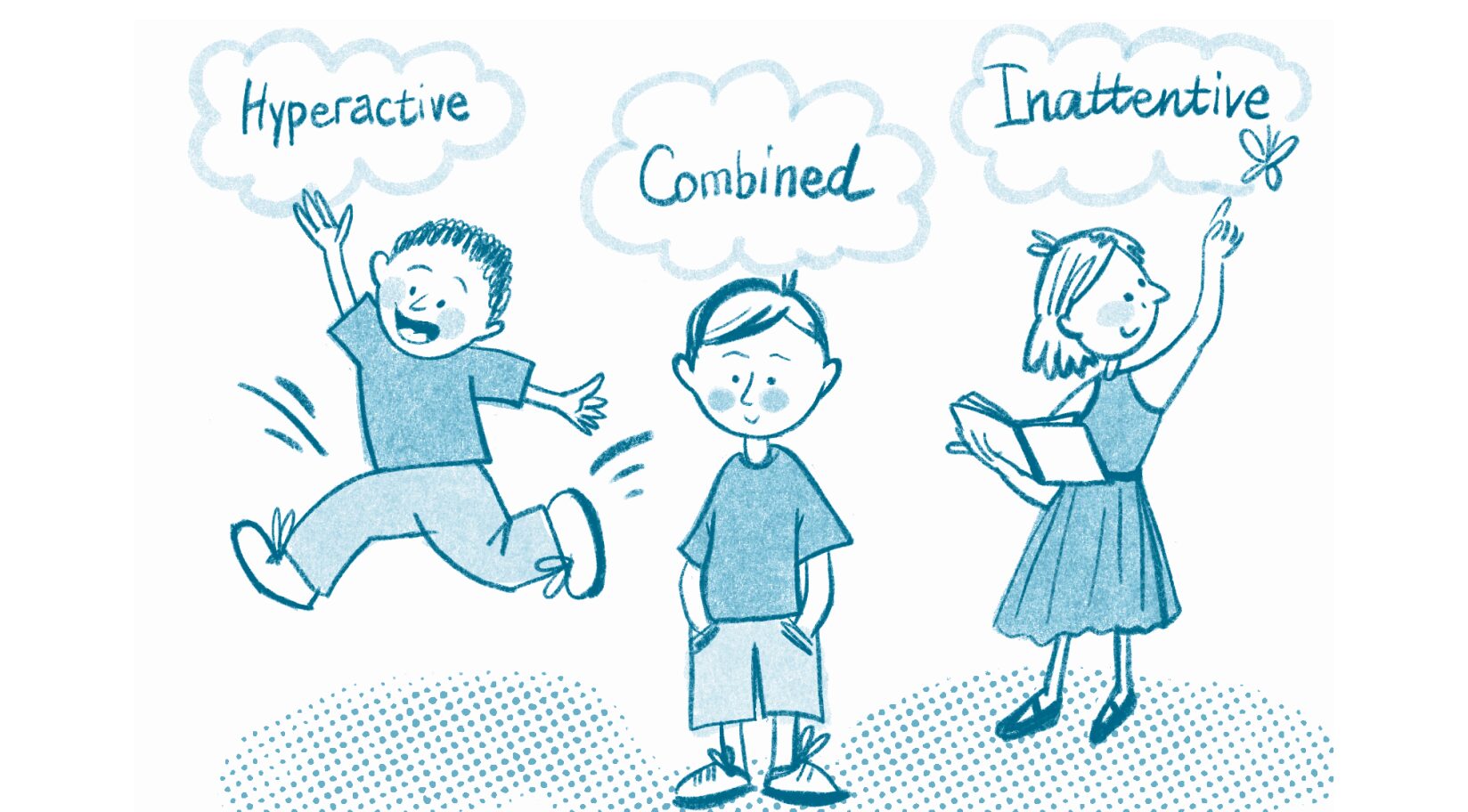
The largest psychiatric organization in the world and the main one in the US, the American Psychiatric Association (APA), created a special Diagnostic and Statistical Manual of Mental Disorders (DSM). The fifth edition of the manual describes three types of ADHD in women, men, and kids, as well as the symptoms for each of them.
Inattentive symptoms of ADHD in children
- Makes careless mistakes and overlooks details.
- Struggles to pay attention to one activity or task.
- Seems to have their mind somewhere else and doesn’t listen even when spoken to directly.
- Fails to organize and finish tasks, as well as follow instructions.
- Is easily distracted.
- Is often forgetful and loses things.
Impulsive-hyperactive symptoms of ADHD in children
- Constantly fidgets with their body parts.
- Struggles to sit or stay still when it’s expected.
- Talks too much.
- Interrupts others, blurts out answers, and struggles to wait their turn.
- Intrudes into others’ activities and takes their things without asking.
Combined ADHD symptoms
It combines the symptoms of both ADHD types and it’s often manifested in more severe forms.
When is it time to diagnose ADHD?

Children can naturally show signs of inattentiveness and hyperactivity at certain ages of their development. However, when these behaviors persist for more than 6 months and the child doesn’t change them upon explanations and structured guidance, it might be time to consider a more thorough evaluation.
This is especially crucial if the behaviors are significantly impacting the ability of your ADHD teenager or child to function in multiple settings, such as at home, in school, and in social environments.
Steps to take toward an ADHD diagnosis:
- Before scheduling an appointment with a doctor:
1.1 Observe the child’s behavior. Parents and teachers should carefully observe the child’s behavior over a period of time. Detailed notes on specific instances of inattention, hyperactivity, and impulsivity can help healthcare providers make a more accurate diagnosis.
It’s important to differentiate ADHD from other conditions that can cause similar symptoms, such as learning disabilities, anxiety disorders, or hearing problems. So, gather information about all the peculiarities of the child.
1.2 Point out the child’s developmental history. Understanding the child’s developmental milestones and any significant events in their life can provide context for their behavior. This also includes looking into family history, as, as we’ve already mentioned, ADHD in girls and boys can be hereditary. - Schedule an appointment with the child’s healthcare provider, a pediatrician, or a mental health professional specializing in ADHD. They’ll diagnose the child and rule out other possible disorders that might better explain the symptoms.
Co-existing conditions
Learning Disabilities (LD)
- Reading disabilities, or dyslexia, are common, making it difficult for children to decode words, read fluently, and comprehend text.
- Math disabilities, or dyscalculia, involve challenges with number-related concepts, mathematical reasoning, and computation.
- Writing disabilities, or dysgraphia, affect handwriting, spelling, and the ability to organize thoughts on paper.
Oppositional Defiant Disorder (ODD)
- Children with ODD display a pattern of anger, irritability, argumentative behavior, and vindictiveness. This can lead to conflicts with authority figures and peers, further complicating ADHD symptoms.
Conduct Disorder (CD)
- CD involves severe behavioral problems such as deliberate aggression towards people and animals, destruction of property, lying, theft, and intentional violations of rules.
Sensory Processing Disorder (SPD)
- SPD involves difficulties in processing and responding to sensory information, leading to over- or under-sensitivity to stimuli such as sounds, textures, and lights. This can result in both behavioral issues and affect daily activities.
How do you treat ADHD in children?
Medications
Stimulant and non-stimulant medications can be prescribed to manage ADHD symptoms. Different types of medications target different neurotransmitters and brain areas. That’s why the decision to use medication should be made only in consultation with a healthcare provider and based on the child’s individual needs.
! Notice that the American Academy of Pediatrics (AAP) recommends starting ADHD medication treatment only if behavioral therapy doesn’t show results.
Behavioral Therapy
Behavioral treatment is used before medications as it tunes the relationships between a child and parents and teaches the child appropriate behavioral strategies. Moreover, for some children, behavioral therapy alone works great, and they don’t need to take ADHD medications at all.
Parenting skills training

Parent training can be the only type of behavioral treatment before the age of six. It’s the most effective approach, as the child can’t yet regulate emotions and impulses independently, and parents play a crucial role in helping them manage their symptoms.
Children with ADHD tend to throw tantrums, exhibit impulsive behavior, are prone to mood disorders, and often develop defiant patterns. Parent education teaches caregivers how to correctly modify children’s behavior and assist them in developing necessary social skills and self-control so that they can function well outside of home.
Parental skills training enables parents to learn how to settle, in a healthy way, consistent consequences for not following rules and instructions in a healthy way. Also, this is where parents can learn about positive reinforcement and how to praise their ADHD children. The problem is that they find themselves scolded much more often than other children, and it can be a risk factor for developing low self-esteem and even some mental health problems.
It’s also beneficial for parents themselves. Often, they get burned out and develop depression because they blame themselves for poor parenting and believe that they’re unable to manage their own children. Behavior therapy can make parenting much more rewarding.
Attention aid
Often, the root of many kids’ underperformance is that they don’t feel time and leave a much shorter period for assignments than is needed. Also, due to poor working memory, they struggle with tasks that require following certain steps, such as bedtime routines and complex sequential projects.
This is why many children with ADHD need structured, precise, and written plans as an aid to their normal functioning. One of the parts of behavior therapy is to teach children and parents how to make and use checklists, reward charts, and daily planners. Doctors recommend limiting time for each task as well as setting timers to teach a child how to manage tasks timely and effectively.
Educational interventions
The teacher must know the diagnosis of your child so that they can accommodate the classroom for them. For instance, teachers will provide more detailed and structured explanations, introduce activities that require a lot of movement, and create an environment with no distractions on the walls. It’s not a whole set of teachers’ adjustments, but it makes a real difference in helping a child succeed academically.
Also, parents can make use of individualized education programs (IEPs). The federal law, the Individuals with Disabilities Education Act (IDEA), orders educational institutions to provide free special education services and support for students with disabilities. They may include:
- an extended time for tests and assignments,
- modifications in curriculum,
- measurable goals (for instance, a student has to complete 80% of tasks on his own by the end of the year),
- attending a speech therapist, social skills training groups, etc.,
- assistance in preparing students for the next steps after high school.
Physical activities
The study has shown that as little as five minutes of jumping improved the symptoms of ADHD in children, while 60–80 minutes of moderate physical activities have proven to be the most beneficial for attention.
Together with releasing excess energy and increasing the amount of neurotransmitters in the brain, sports build the physical well-being of a child, facilitating normal muscle and skeleton development.
Can an ADHD child lead a normal life?
Sure! When diagnosed early, the child, with the aid of their parents and educators, develops coping strategies and healthy behaviors that improve their functioning and enhance their quality of life. Basically, it’s almost the same as bringing up neurotypical children, but ADHD requires a different approach that should be learned.
ADHD kids require attention and care. Remember that as a parent, you are your child’s first and biggest source of inspiration and motivation. Check out our list of understanding ADHD quotes you can share with your kid.
Managing the disorder is an ongoing process both for ADHD adults and kids. Regular follow-ups with healthcare providers to monitor the child’s progress and adjust treatment plans are essential. But be sure, the earlier you start the right treatment, the easier the life of the child is going to be.